Medical Case Study - A Cystic Fibrosis Case Study
When you go to the hospital, it always looks like your doctor is relying on illness script to diagnose you being that they have to look at characteristics associated with the patient which would include the age, geographical location, and symptoms but these is different when a differential diagnosis is in play because they need to keep an open mind. In this post, I want us all to be online physicians and doctors, let's both go through this case and find out what could be wrong with this patient. This is a case study published in The New England Journal of Medicine.
This is a case of a 42 year old woman Chinese woman who immigrated to the United States about 10 years ago presented to the emergency room with severe cough and shortness of breath (Dyspnea). She had beeen experiencing shortness of breath, fatigue, thick cough that came with yellow-green sputum. When the doctor asked her to explain what had been going on with her, she was able to tell that she has been experiencing low-grade fevers and chills.

The doctors asked about any travel and who she lived with, and the woman replied that she lived with her husband and 2 children, she had no pets, she had not traveled in recent times, and she had no contact with any sick person. When she was asked about lifestyle habits, she didn't use tobacco, or smoke any thing.
Dyspnea could be as a result of some health challenges including pulmonary causes such as Pneumonia, hematological causes such as Anemia, Metabolic causes such as Ketoacidosis, Cardiac causes such as heart failure, other reasons can be Anxiety (psychiatry), and Myasthenia gravis (neuromuscular). But in this case of the woman, the dyspnea is accompanied with fever and purulent cough which is a sign of an infection and in this case, a pulmonary infection so we could assume that it is an infectious pneumonia.
If it is an infectious pneumonia, what could be the possible cause. Viruses such as the SARS-CoV2, and Influenza, as well as gram positive and negative bacteria can be the cause, and fungi such as Pneumocystis jirovecii can cause it. We could also be careful to not rule a chance of it being Mycobacterium tuberculosis or a case of a reactivated parasitic infection.
When patient's body stat was checked, it was seen that her temperature was at 38.4oC which means she was febrile, her heart rate was high at 122 beats per minute showing she was tachycardic, respiration rate at 38 breaths per minute (tachypneic), blood rate low at 93/65 mm Hg (Hypotensive), and she was hypoxemic. The patient was placed on oxygen of 4 liters per minutes as she wasn't getting enough oxygen.
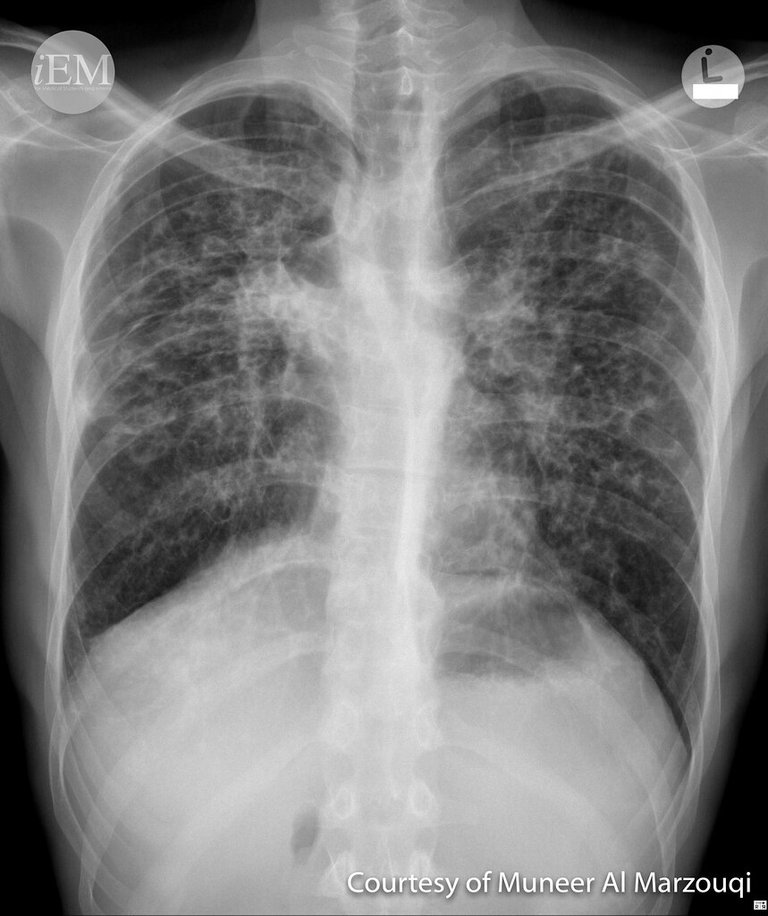
Standard lab work was done, and results showed that she had an elevated white blood cell of 26000 per cubic millimeter, elevated bicarbonate, and elevated glucose level. Test for influenza type A and B and SARS-CoV2 came back negative and liver enzyme were normal. A chest X-ray was done and and it suggested that the airways was wide and thick, which suggested Bronchiectasis which can be associated with cough, sputum. Possible cause of this would include common variable immunodeficiency, Cystic fibrosis, Alpha-1 antitrypsin deficiency, COPD, Aspiration, or even HIV. Chances are that it could be Rheumatoid Arthritis, and Systemic lupus erythematosus. In some cases, there could be no cause and this is referred to as Idiopathic Bronchiectasis.

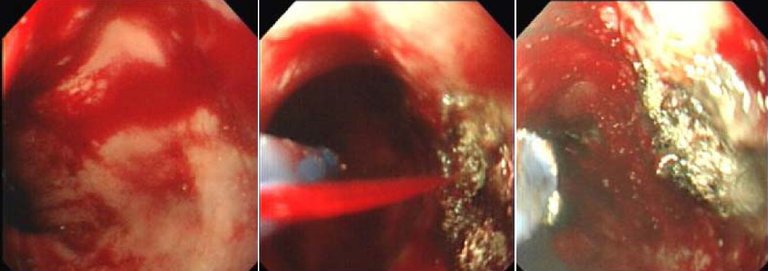
The patient was started on Broad Spectrum Antibiotics Vancomycin and Cefepime but her condition continued to worsen. Her Arterial blood gas was checked and it showed a high partial pressure of CO2 at 88mm Hg and a low pH d 7.20. The patient was suffering from Acute and Chronic respiratory Acidosis. This showed that her kidneys were holding up to Bicarbonate as her bicarbonate levels were high as a result of increased carbon dioxide in blood. The patient was placed on a ventilator as a result of hypoxemic and hypercarbic respiratory failure but as the failure worsened, she had to be intubated and in the process, yellow secretion mixed with blood were seen in her airway which lead to another x-ray after the intubation and this showed a right apical pneumothorax and so a thoracostomy tube was placed.
The patient was treated with with Norepinephrine and vasopressin, also empiric antituberculosis therapy including Rifampin, Isoniazid, Ethambutol, and Pyrazinamide were added to her antibiotic regime even when there was no disease evidence disseminated on the chest image but it was necessary to give this treatment.
Other tests were done such as HIV, Alpha-1 antitrypsin deficiency, Antinuclear antibofy titer, Aspergillus antigen and Antibodies, and Rheumatoid factor were all negative but her blood glucose was still high so she was placed on insulin therapy to help with that. In all this, the patient was still experiencing respiratory failure and this gave the option of a cystic fibrosis.
With genetic testing for cystic fibrosis, one could confirm if it is the cause for the continuous respiratory failure. When culture returned after three weeks, it returned with Mycobacterium avium intracellulare complex, as well as mycobacterium abscesses subspecies bolletti. She was treated with Rifampin, Ethambutol, Azithromycin, Linezolid, Imipenem, and Amikacin. So the patient result from the Cystic Fibrosis transmembrane conductase regulator (CFTR) showed a nucliec acid variant c.293A->G and another variant c.2936A->C was also seen.
Cystic fibrosis happens as a result of dysregulated ion transport due to defects in the CFTR protein which are of 5 classes. When a person suffers from cystic fibrosis they experience Bronchiectasis, Exocrine and Endocrine Pancreatic insufficiency, Colonic obstruction, and infertility. treatment began after she was diagnosed with Cystic Fibrosis but not with with CFTR modulators tezacaftor-ivacaftor, Elexacaftor-tezacaftor-ivacaftor as they had not been approved by the FDA as at the time but she was treated with off-label therapy with ivacaftor even when it had not been approved. She suffered recurrent pulmonary infection with septic shock, and progressive respiratory failure for months and this led to her death.
Post Reference
https://www.nejm.org/doi/full/10.1056/NEJMcps2214685
https://www.nhlbi.nih.gov/health/bronchiectasis
https://www.nhs.uk/conditions/bronchiectasis/
https://my.clevelandclinic.org/health/diseases/21144-bronchiectasis
https://www.nhlbi.nih.gov/health/cystic-fibrosis
https://www.cdc.gov/cystic-fibrosis/about/index.html
https://emedicine.medscape.com/article/1001602-overview
https://www.uptodate.com/contents/cystic-fibrosis-treatment-with-cftr-modulators
https://www.cff.org/managing-cf/cftr-modulator-therapies
IMAGE REFERENCE
Image 1|| Wikimedia Commons || Skillslab endotracheale-intubation
Image 2|| Wikimedia Commons || APC oesophagus
Image 3|| freemalaysiatoday || Ventilators are in short supply in many countries hardest hit by Covid-19
Image 4|| Flickr || cyctic fibrosis 1
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.